Advice for medical practitioners
Advice for medical practitioners
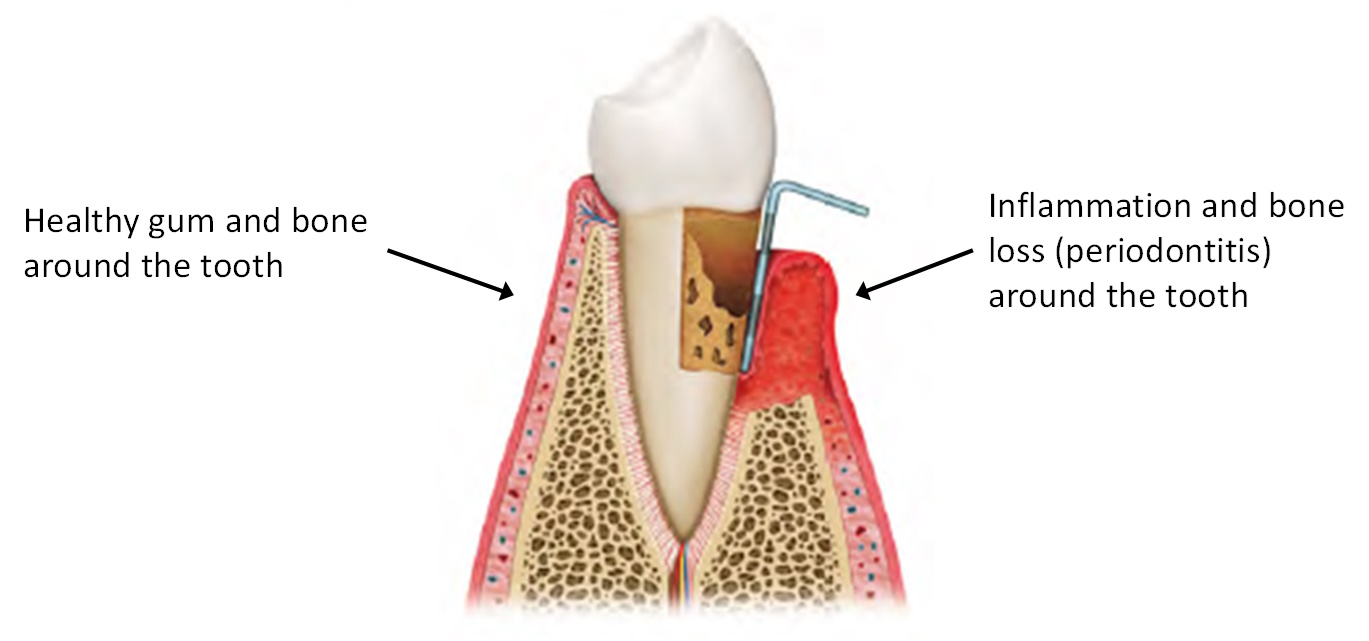
Periodontal (gum) diseases are a group of related conditions, both acute and chronic, that affect the soft tissues and bone holding the teeth in place. In most cases these are primarily diseases associated with plaque micro-organisms present on the teeth which, in the early stages, cause local, reversible damage to soft tissues (gingivitis) and, at later stages, irreversible damage to the bone holding teeth in place (periodontitis). This loss of bone can lead to loss of teeth if undiagnosed and untreated in patients who are susceptible. Tooth loss is associated with reduced function and quality of life and impaired nutrition. In addition there is evidence that periodontal diseases have a systemic effect, increasing inflammation and activating immune mechanisms.
Differences in supporting tissues in health and periodontitis
Several medical conditions (e.g. diabetes) and social factors (e.g. smoking) put patients at higher risk of developing periodontal diseases. In addition, emerging evidence links periodontitis with a raised risk of developing or worsening existing systemic conditions.
Patients with type 1 and type 2 diabetes have a higher risk of developing periodontal (gum) disease. This is particularly true for patients whose diabetes is sub-optimally controlled. There is also evidence that periodontal treatment of patients with diabetes can lead to improved glycaemic control. This connection is recognised in the NICE guidelines on management of type 1 diabetes (NG17)22 and type 2 diabetes (NG28),23 and advice for the medical team in relation to diabetes and oral health is provided there.
Patients with diabetes should be advised to maintain good oral hygiene to both minimise their risk of periodontal disease and help control their diabetes.
Advise patients with diabetes:
- that their condition is associated with a higher risk of periodontal (gum) disease;
- to make an appointment with a dentist as soon as possible for a full oral assessment;
- to tell their dentist that they have diabetes.
N.B. Patient leaflets, which provide information about the link between diabetes and oral health, can be found in Supporting tools.
Certain types of medication can lead to gingival enlargement in some patients. These medications include calcium channel blockers, phenytoin and ciclosporin. This gingival enlargement can become unsightly, can limit chewing and comfort and the tissue is often inflamed. While good oral hygiene can limit the risk of gingival enlargement, some patients are particularly susceptible to the problem. In these situations, the dental team will initially try to control inflammation and the patient’s symptoms but may contact you to discuss modification of the drug regimen.
Advise patients taking these medications:
- that a possible side effect of the medication is gingival enlargement;
- to make an appointment with a dentist as soon as possible for a full oral assessment;
- to tell their dentist that they are taking the medication.
The changes in hormone levels and to the immune response associated with pregnancy have been implicated in the development or worsening of gingivitis (superficial inflammation of the soft tissues around the teeth). This manifests as bleeding, swollen gums and can be painful. If the problem is limited to the soft tissues then good homecare and oral hygiene, with support from the dental team should resolve this. Most cases will resolve on delivery of the baby, although breastfeeding can extend the duration of the condition.
Advise pregnant patients:
- that they may experience red, swollen and bleeding gums during their pregnancy;
- to make an appointment with a dentist as soon as possible for a full oral assessment.
More severe periodontal disease, involving bone loss around teeth, has been linked with adverse pregnancy outcomes, such as pre-term birth and low birth weight. The nature of this relationship is complex and co-morbidities such as smoking may be important. The impact of periodontal treatment on adverse pregnancy outcomes is unclear but it is acknowledged that periodontal treatment is safe during pregnancy.
Gingivitis is commonly observed in pre-teens and young teenagers where the increased inflammatory response to plaque is thought to be aggravated by the hormonal changes associated with puberty. Gingival enlargement may also be observed in susceptible individuals.
Non-plaque biofilm-induced periodontal diseases (e.g. lichen planus) are a less common group of conditions not directly caused by dental plaque characterised by atypically presenting gingival, and sometimes oral mucosal, lesions.94 They may be manifestations of systemic conditions, a medical disorder or may represent pathologic changes in the gingival tissues. Their atypical appearance will often extend beyond the mucogingival margin and will not respond to oral hygiene measures prescribed by a dental team.
If a medical practitioner is unsure about the nature of the oral condition, early referral to a general dental practitioner should be considered to confirm a diagnosis.
Links between periodontal diseases and other non-communicable diseases (NCDs) such as cardiovascular disease, rheumatoid arthritis, chronic kidney disease and Alzheimer’s disease have been suggested. Common factors linking periodontal disease and NCDs relate to systemic inflammation. Treatment to control periodontitis leads to reductions in local and systemic inflammation but, with the exception of diabetes, it is unclear whether this leads to improved systemic disease outcomes. Periodontal treatment is safe in patients with NCDs and patients should be encouraged to attend the dentist for treatment.
Systemic conditions which may increase the risk of periodontal diseases include stress, diet, and obesity. The mechanisms for this are unclear but patients should be encouraged to adopt a healthy lifestyle.
A significant proportion of the population only seek dental care when they suffer an acute episode and may initially present to other providers of care (e.g. general medical practitioner, accident and emergency, pharmacy). Advice on dealing with acute dental problems can be found in the SDCEP Management of Acute Dental Problems guidance.137
To help find a dentist in Scotland, patients can consult Scotland's Service Directory via NHS Inform or by contacting their local NHS Health Board.