Engagement
Determining who will benefit from further treatment
It is important that at all stages where decisions about further active treatment or periodontal maintenance are made, there is a discussion with the patient about their particular situation. The implications of further active treatment, no treatment, or maintenance should be made clear, with the patient’s wishes considered during any decisions.
An important component of assessment is to gauge which patients are likely to benefit from more advanced treatment, such as surgery or repeated subgingival PMPR. Treatment outcomes following periodontal therapy are related to several factors, including the level of plaque control which can be achieved by the patient and their ability or desire to attend for and engage with treatment.
The BSP implementation of European S3 – level evidence-based treatment guidelines for stage I-III periodontitis in UK clinical practice (BSP-S3)6 guideline groups these patient factors as ‘engagement’ and states that this is a key principle to consider in periodontal diagnosis, planning and treatment provision when determining who may benefit from further treatment. As part of assessing engagement, the guideline includes a guide outlining levels of plaque and marginal bleeding which may indicate that the patient is engaged, particularly where more advanced treatment is being considered. These are:
- plaque levels of ≤20% and marginal bleeding levels ≤30%, or
- ≥50% reduction in plaque and marginal bleeding from baseline measurements.
Alternatively, targets for improvements in plaque and marginal bleeding levels can be agreed by the patient and clinician.
While Step 1 of therapy should be provided in all circumstances, the BSP-S3 guideline suggests that only those patients who are engaging will benefit from further treatment (Steps 2-4 of therapy). Resolution of periodontal inflammation is unlikely without adequate plaque control. Therefore, where oral hygiene does not initially improve sufficiently, focussing on improving the patient’s plaque control (i.e. repeating Step 1), with the hope that this will in time allow further treatment to be successfully provided, may be appropriate. However, in some cases, it is acceptable to continue to Step 2 of treatment if subgingival PMPR is required to control inflammation. If this is the case, continued support for improved oral hygiene remains important.
Assessing engagement
The management of periodontal diseases relies on teamwork between the dental team and the patient. For this team to function well, both the patient and the dental team need to be engaged in the process of changing behaviour and modifying risk factors to promote health. The dental team are responsible for diagnosing the problem and ensuring that the patient understands what is wrong, knows what is advised to control the problem and has the required skill and support. The patient needs to take responsibility for controlling modifiable risk factors by altering behaviours which put them at risk and attending for treatment as agreed.
While good oral hygiene is key to resolving inflammation and maintaining treatment benefits, oral hygiene is a skill and not purely an indicator of psychological motivation and desire for treatment. The necessary skill of oral hygiene relies not only on the patient’s motivation to improve but also on their capability and opportunity to conduct good oral hygiene behaviours. In addition, the role of the dental team must be considered, for example their ability to explain the diagnosis and its implications, and to ensure that the patient knows what their own role in the treatment process entails. Finally, the dental team should support the patient to control risk factors in a way that allows the patient to play an active part in their treatment.
In light of this, a broad and holistic view of patient engagement based on the principles of behaviour change may be appropriate. Principles of behaviour change management suggest that the complex process of long-term change of habits needed for patients with periodontal diseases requires more than a simple conversation with an individual. This is discussed further in the Public Health England publication Achieving Behaviour Change. A guide for local government and partners (2019).88
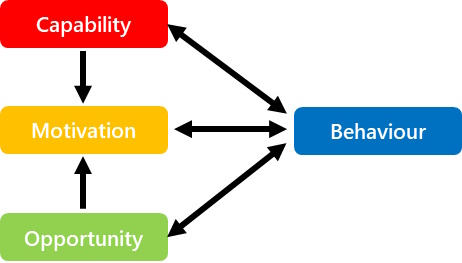
A commonly used model to understand the factors influencing an individual’s behaviour is the COM-B model.89 This model proposes that for a behaviour to occur, an individual must have the Capability, Opportunity and Motivation to perform the Behaviour. Not only do these factors influence behaviour, they also can influence each other, for example motivation may increase if capability is increased.
The COM-B model of behaviour encompasses the following components:
Capability: the physical or psychological capability to perform the behaviour. This can include the knowledge of how to perform the behaviour, the understanding that the behaviour is important, or the physical skills to perform the behaviour.
Opportunity: the physical or social opportunity to perform the behaviour. This can include considerations of the environment, availability of resources (including cost of treatment), social influences or cultural norms.
Motivation: the motivation to perform the behaviour. This can include desire, intention and personal beliefs that may influence the decision to perform the behaviour.
The COM-B model of behaviour
The table below presents some relevant questions to consider for each of the three components of the COM-B model. These questions can be used to reflect on the ability of the patient to perform a behaviour, such as oral hygiene, and the ability of the clinician to support the patient.
Examples of questions related to influences on patient and clinician behaviour
| Patient behaviour | Clinician behaviour | |
| Capability |
|
|
| Opportunity |
|
|
| Motivation |
|
|
To promote patient engagement in treatment, clinicians can use one or multiple aspects of the COM-B model to help support patients to change their behaviour, when the patient is ready to change. In addition, clinicians can use the COM-B model to consider their own behaviour in relation to supporting the patient to adopt and maintain a new behaviour.
This holistic approach to assessing patient engagement, considering the capability, opportunity and motivation of both patient and clinician, may help to identify engaging patients who are not currently able to achieve the levels of plaque and bleeding specified by the BSP-S3 guideline, but who, with further support, may be able to achieve this in time.
Further information regarding the principles of behaviour change can be found in the Delivering Better Oral Health toolkit.7
Note that even in the absence of adequate plaque control to proceed to Steps 2 or 3 of treatment, periodontal charting, and recording of that charting, should be carried out in accordance with guidance where BPE scores of 3 or 4 are measured or where a diagnosis of periodontitis has been made (see Periodontal assessment).