Assessing tooth prognosis
Assessing tooth prognosis
Before detailed planning of periodontal care commences, the teeth and dentition as a whole should be assessed with regard to tooth prognosis, the potential retention or loss of teeth and the benefits to be gained by providing treatment (see figure: Assessing tooth prognosis). This assessment is accompanied by a discussion with the patient about which teeth may be reliably retained, which teeth are more likely to need complex management, and which are at risk of being lost. Many teeth of uncertain prognosis can be retained in the early stages of management (in agreement with the patient), with their longer-term retention considered at a later stage.
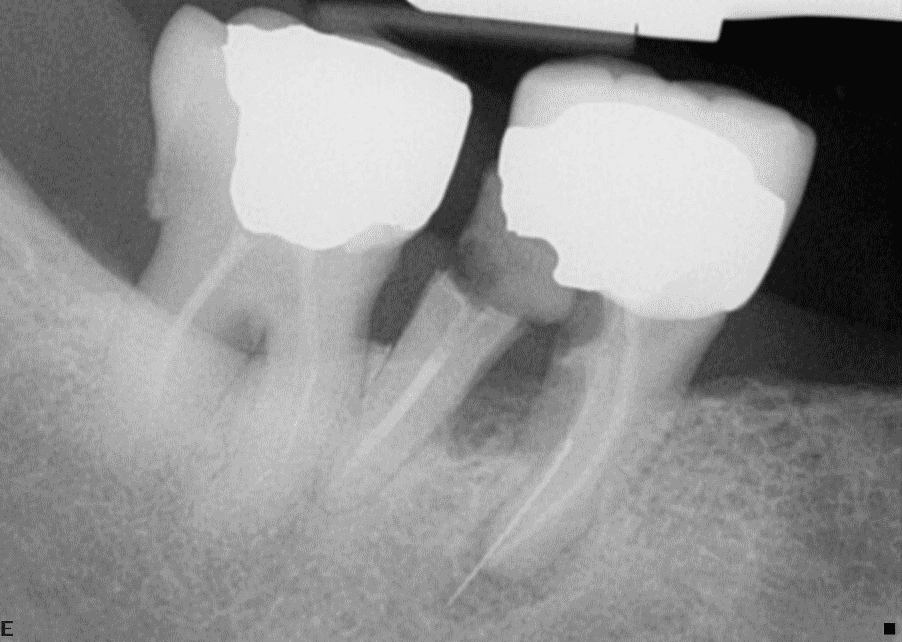
Tooth 47 is affected by periodontitis extending into the furcation, is heavily restored and has an inadequate root filling. Tooth 46 has Stage III periodontitis with a Grade III furcation lesion, extensive caries beneath a full coverage crown and a mesial periapical radiolucency. Tooth 46 is unsaveable due to the multiple problems and the extent of caries and periodontitis when considered together. However, despite its compromised prognosis, tooth 47 may be useful tooth to retain following periodontal and endodontic treatment if there is a need or a desire to avoid a free end saddle situation or to provide distal occlusal support.
Assessment of tooth prognosis includes consideration of factors which are likely to affect the ability to successfully control periodontal disease, along with factors related to the condition and site of the tooth itself. It also takes into consideration the likelihood of stabilising the tooth so that it can be maintained in a functional way. The assessment of tooth prognosis is not straightforward and current research suggests that parameters for determining tooth prognosis may not accurately predict the chance of successful treatment.
Prognosis is an ongoing, dynamic process and the following factors can be considered at different stages of management.
- Patient related factors, for example:
- oral hygiene (which may change in response to motivation and education);
- the presence of systemic risk factors (e.g. smoking or diabetes);
- behavioural and biological response to treatment.
- Tooth related factors, for example:
- the degree of bone support;
- probing pocket depth;
- the presence of furcations, root grooves or dental anomalies;
- the presence of periapical pathology;
- the presence of large restorations or caries;
- tooth position and occlusion;
- pulp vitality;
- the strategic value of the tooth.
Consider the strategic value of periodontally-involved teeth when assessing management options.
Assess the prognosis of periodontally-involved teeth, taking into account tooth-related factors (e.g. furcation involvement, pulpal status, periapical status, the presence of restorations/caries, tooth position) and patient-related factors (e.g. risk factors, patient preferences, access to specialist support).
Consider advising the extraction of teeth which are unrestorable, impairing function (e.g. hypermobile where splinting or occlusal management is not possible) or persistently infected despite treatment (i.e. periodontitis or endodontic abscess).
- Note that some severely affected teeth can often be retained successfully for many years.