Treatment of peri-implantitis
Treatment of peri-implantitis
Peri-implantitis is defined as a pathological condition occurring in tissues around dental implants, characterized by inflammation in the peri-implant mucosa and progressive loss of supporting bone.114 The tissues will appear red and swollen, bleed on gentle palpation or probing and there may be suppuration (see figure: Peri-implantitis). Soft tissue inflammation is detected by probing (bleeding on probing indicates the presence of inflammation), while progressive bone loss is identified on radiographs. Recession of the surrounding mucosa can occur, exposing the implant threads. Peri-implantitis can progress rapidly. The patient may also experience pain around the implant. However, this usually only occurs during episodes of acute infection.
The goals of treatment are residual peri-implant probing depths of ≤5 mm, BOP at ≤1 site (bleeding should not be profuse) and absence of suppuration around the affected implant.10
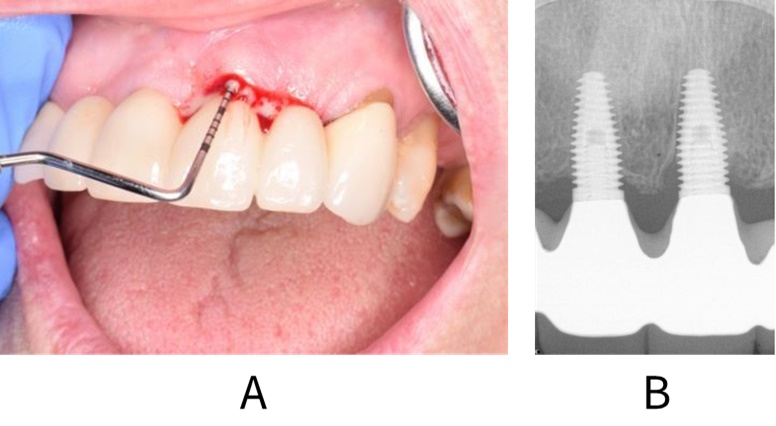
Clinical (A) and radiographic (B) images showing peri-implant inflammation and bone loss in a patient with peri-implantitis.
Key recomendations
For patients with peri-implantitis, the routine use of adjunctive or alternative measures to professional mechanical plaque removal is not recommended.
(Conditional recommendation; low certainty evidence)
The routine use of local or systemic antibiotics for the treatment of peri-implantitis in primary care is not recommended.
(Conditional recommendation; low certainty evidence)
A consensus statement from the World Dental Federation noted that conventional non-surgical professional mechanical plaque removal (PMPR) may result in short-term improvements in inflammatory parameters but is unlikely to resolve the disease.124 Evidence suggests that specific alternative or adjunctive therapies, such as antiseptics, antibiotics or treatment using lasers, do not significantly improve clinical outcomes when compared with PMPR alone.127-133 The certainty of the evidence ranges from moderate to low due to factors such as risk of bias, inconsistency and small study sizes.
Non-surgical interventions to manage peri-implantitis (i.e. the re-establishment of effective self-performed oral hygiene and professional removal of supra- and submucosal plaque biofilm and calculus deposits and excess residual cement) may be helpful in the initial stages of treatment to reduce inflammation and pathogenic microbiota.124, 131
The EFP Prevention and treatment of peri-implant diseases guideline10 recommends initial non-surgical management. This includes oral hygiene instruction and motivation, risk factor control, prosthesis cleaning/removal/modification (including controlling biofilm retentive factors and evaluation of the components of the prosthesis where required and feasible), and supramucosal and submucosal PMPR around the implant. In addition, where periodontal disease is present elsewhere in the mouth, this should be treated. PMPR around the implant can be performed with ultrasonic or sonic devices or hand instruments. The guideline suggests not to use air polishers, lasers, photodynamic therapy, antiseptic gel or probiotics as monotherapies or as adjuncts to PMPR. Regarding antimicrobial therapy, the guideline does not recommend the use of systemic antibiotics as adjuncts to PMPR and suggests not to use locally administered antimicrobials as an adjunct to PMPR or as a monotherapy.
Further details on the development of the recommendations in this guidance can be found in Methodology.
The management of peri-implantitis is difficult and unpredictable and surgical management is often required.* However, even this may not be sufficient to control the disease and in cases where there is progressive bone loss around the implant, implant removal may be a valid management option. Initial non-surgical options around implant-supported restorations can be challenging to deliver and referral to the clinical team which placed the implants, especially where complex restorations are present, may be appropriate if peri-implantitis develops.
It is recognised that referral for management of peri-implantitis may either not be possible (e.g. for example the clinical team that placed the implant cannot provide ongoing maintenance care) or may not be straightforward (e.g. local services to support the patient post-placement may not be available). In these cases, the primary care team is encouraged to provide treatment and support, within their skill mix where possible, and on an ongoing basis.
*While surgical management of peri-implantitis is often indicated, this is beyond the scope of the guidance and specific aspects and techniques will not be discussed here.
If soft tissue inflammation is present:
Carry out a radiographic examination of the implant using periapical radiographs, taken using the long cone paralleling technique, to evaluate peri-implant bone levels compared with the baseline radiograph.
If progressing crestal bone loss is detected, refer back to the clinician who placed the implant.
- Surgical management may be considered in these cases.
If referral is not possible, consider whether the implant is saveable. For example, 80% bone loss around the implant indicates that it is likely to fail in the short-term.
- If it is not clear whether the implant is saveable, discuss the situation with the patient and review the options for referral.
If the implant is saveable, carry out initial non-surgical management.
- Check the restoration contour to ensure that patient performed oral hygiene is possible. If the restoration does not allow access for home care, consider whether it is possible to recontour or replace the restoration to allow adequate oral hygiene.
- Check for the presence of retained cement around the restoration.
- Provide personalised oral hygiene advice and instruction to assist and encourage the patient to improve their oral hygiene skills as well as their understanding of the value of good self-care routines (see Oral hygiene).
- Encourage the use of implant-specific oral hygiene aids such as implant floss and interdental brushes.
- Where applicable, give smoking cessation advice and support (see Smoking cessation).
- Remove supramucosal and submucosal plaque and calculus and any retained cement using an appropriate method. Local anaesthesia may be required.
- If access for debridement is difficult, and there are indications not to remove the restoration, consider the use of adjunctive or alternative therapies.
- Arrange a follow-up appointment after 1-2 months to assess the outcome of treatment. Re-examine the peri-implant tissues. Where there is no improvement or in the presence of acute pain and infection, seek advice from secondary care.
- If referral to secondary care is not possible and there is persistent inflammation, discuss the situation with the patient, repeat non-surgical management and review the options for referral. In some cases, the only option may be for the primary care team to provide care to control symptoms and superficial inflammation around the implant.
- If the inflammation has settled, arrange radiographic follow-up in 6-12 months to check crestal bone levels. If bone loss is ongoing, seek advice from secondary care.
- Ensure regular, risk-based recall for maintenance of the implants and their restorations is arranged.