Dental implants
Management of patients with dental implants
There are several treatment options when patients lose teeth; these include dental implants and the more conventional options of fixed bridgework, dentures or leaving the space unrestored.
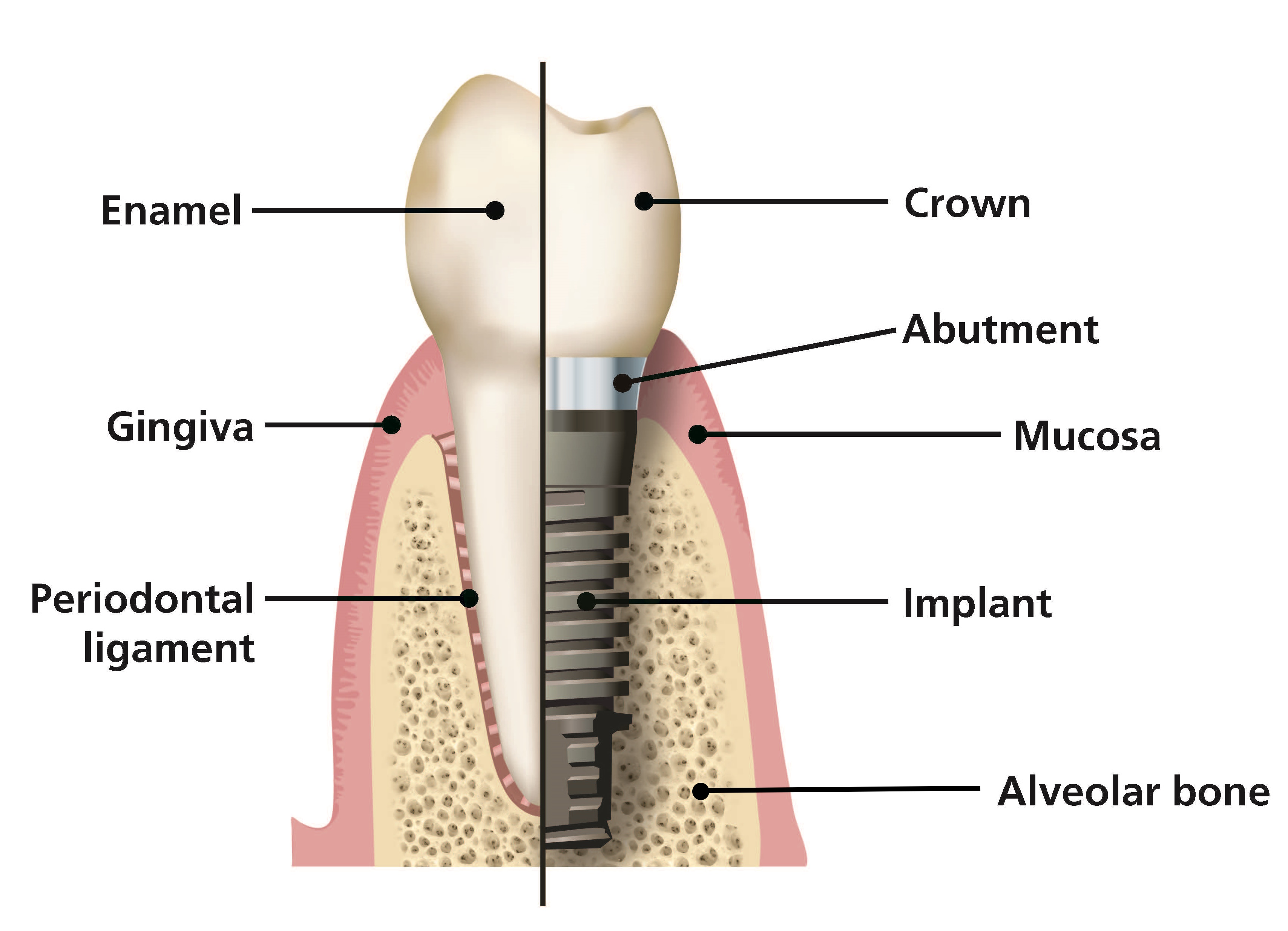
Dental implants are surgical, titanium, screw-like devices placed directly into bone either immediately after a tooth is extracted or after bone has healed. After placement, bone grows directly onto the titanium surface and leads to osseointegration of the implant. In most cases, once this process is complete the implant is loaded, by attaching a restoration to it, and the implant/restoration combination will function much like a natural tooth. In some selected cases, implants are loaded immediately after placement. The principal difference between a tooth and an implant is that between tooth and bone there is a periodontal ligament whereas there is a direct connection between an implant and bone (as shown in figure: Anatomical differences between tooth and implant).
Anatomical differences between tooth and implant
Like teeth, implants are susceptible to the effects of bacterial plaque and calculus formation, leading to an inflammatory response in the peri-implant tissues, either superficially in the mucosa or more deeply in the bone. Peri-implant tissues can also become inflamed in response to the presence of a foreign body, such as excess residual cement which may be present if an implant restoration is cemented rather than screwed in place.
Peri-implant disease is known to be multi-factorial and both biological and non-biological factors increase the risk of the disease and implant loss. The reported prevalence of peri-implant disease is variable, mainly due to the variation in definitions of the disease used in different studies but is estimated to affect approximately 20% of patients and 11.5% of implants overall.110